White blood cells, or leukocytes (also spelled "leucocytes"; from the Greek word leuko- meaning "white"), are cells of the immune system involved in defending the body against both infectious disease and foreign materials. Five different and diverse types of leukocytes exist, but they are all produced and derived from a multipotent cell in the bone marrow known as a hematopoietic stem cell. They live for about 3 to 4 days in the average human body. Leukocytes are found throughout the body, including the blood and lymphatic system.
Etymology
The name "white blood cell" derives from the fact that after centrifugation of a blood sample, the white cells are found in the buffy coat, a thin, typically white layer of nucleated cells between the sedimented red blood cells and the blood plasma. The scientific term leukocyte directly reflects this description, derived from Ancient Greek λευκό (white), and κύτταρο (cell). Blood plasma may sometimes be green if there are large amounts of neutrophils in the sample, due to the heme-containing enzyme myeloperoxidase that they produce.
Types
There are several different types of white blood cells. They all have
many things in common, but are all distinct in form and function. A
major distinguishing feature of some leukocytes is the presence of granules; white blood cells are often characterized as granulocytes or agranulocytes:
- Granulocytes (polymorphonuclear leukocytes): leukocytes characterised by the presence of differently staining granules in their cytoplasm when viewed under light microscopy. These granules are membrane-bound enzymes that act primarily in the digestion of endocytosed particles. There are three types of granulocytes: neutrophils, basophils, and eosinophils, which are named according to their staining properties.
- Agranulocytes (mononuclear leukocytes): leukocytes characterized by the apparent absence of granules in their cytoplasm. Although the name implies a lack of granules these cells do contain non-specific azurophilic granules, which are lysosomes. The cells include lymphocytes, monocytes, and macrophages.
Neutrophil
Neutrophils defend against bacterial or fungal
infection and other very small inflammatory processes that are usually
first responders to microbial infection; their activity and death in
large numbers forms pus.
They are commonly referred to as polymorphonuclear (PMN) leukocytes,
although, in the technical sense, PMN refers to all granulocytes. They
have a multi-lobed nucleus that may appear like multiple nuclei, hence
the name polymorphonuclear leukocyte. The cytoplasm may look transparent
because of fine granules that are pale lilac. Neutrophils are very
active in phagocytosing bacteria and are present in large amount in the
pus of wounds. These cells are not able to renew their lysosomes (used in digesting microbes) and die after having phagocytosed a few pathogens.
Neutrophils are the most common cell type seen in the early stages of
acute inflammation, and make up 60-70% of total leukocyte count in human
blood. The life span of a circulating human neutrophil is about 5.4 days.
Eosinophil
Eosinophils primarily deal with parasitic
infections. Eosinophils are also the predominant inflammatory cells in
allergic reactions. The most important causes of eosinophilia include
allergies such as asthma, hay fever, and hives; and also parasitic
infections. In general, their nucleus is bi-lobed. The cytoplasm is full
of granules that assume a characteristic pink-orange color with eosin
stain.
Basophil
Basophils are chiefly responsible for allergic and antigen response by releasing the chemical histamine causing vasodilation.
The nucleus is bi- or tri-lobed, but it is hard to see because of the
number of coarse granules that hide it. They are characterized by their
large blue granules.
Lymphocyte
Lymphocytes are much more common in the lymphatic system. Lymphocytes
are distinguished by having a deeply staining nucleus that may be
eccentric in location, and a relatively small amount of cytoplasm. The
blood has three types of lymphocytes:
- B cells make antibodies that bind to pathogens to enable their destruction.
- T cells:
- CD4+ helper T cells: T cells having co-receptor CD4 are known as CD4+ T cells. These cells bind antigen presented by antigen-presenting cells via T-cell receptor interacting with MHC II complex on APC. Helper T cells coordinate the immune response. In acute HIV infection, these T cells are the main index to identify the individual's immune system activity.
- CD8+ cytotoxic T cells: T cells having co-receptor CD8 are known as CD8+ T cells. These cells bind antigens presented on MHC I complex of virus-infected or tumour cells and kill them. All nucleated cells possess MHC I on its surface.
- γδ T cells possess an alternative T cell receptor as opposed to CD4+ and CD8+ αβ T cells and share characteristics of helper T cells, cytotoxic T cells and natural killer cells.
- Natural killer cells are able to kill cells of the body that have lost MHC I molecule, as they have been infected by a virus or have become cancerous.
Monocyte
Monocytes share the "vacuum cleaner" (phagocytosis) function of neutrophils, but are much longer lived as they have an additional role: they present pieces of pathogens
to T cells so that the pathogens may be recognized again and killed, or
so that an antibody response may be mounted. Monocytes eventually leave
the bloodstream to become tissue macrophages, which remove dead cell
debris as well as attacking microorganisms. Neither of these can be
dealt with effectively by the neutrophils. Unlike neutrophils, monocytes
are able to replace their lysosomal
contents and are thought to have a much longer active life. They have
the kidney shaped nucleus and are typically agranulated. They also
possess abundant cytoplasm.
Once monocytes move from the bloodstream out into the body tissues, they undergo changes (differentiate) allowing phagocytosis and are then known as macrophages.
Medication causing leukopenia
Some medications can have an impact on the number and function of white blood cells. Leukopenia
is the reduction in the number of white blood cells, which may affect
the overall white cell count or one of the specific populations of white
blood cells. For example, if the number of neutrophils is low, the condition is known as neutropenia. Likewise, low lymphocyte levels are termed lymphopenia. Medications that can cause leukopenia include clozapine, an antipsychotic
medication with a rare adverse effect leading to the total absence of
all granulocytes (neutrophils, basophils, eosinophils). Other
medications include immunosuppressive drugs, such as sirolimus, mycophenolate mofetil, tacrolimus, and cyclosporine. Interferons used to treat multiple sclerosis, like Rebif, Avonex, and Betaseron, can also cause leukopenia.
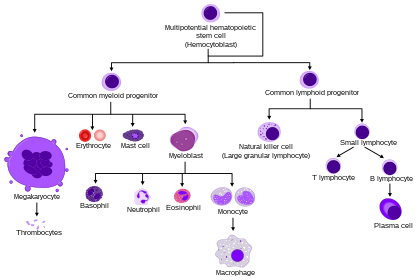
Fixed leukocytes
HSC=Hematopoietic stem cell, Progenitor=Progenitor cell, L-blast=Lymphoblast, Lymphocyte, Mo-blast=Monoblast, Monocyte, Myeloblast, Pro-M=Promyelocyte, Myelocyte, Meta-M=Metamyelocyte, Neutrophil, Eosinophil, Basophil, Pro-E=Proerythroblast, Baso-E=Basophilic erythroblast, poly-E=Polychromatic erythroblast, Ortho-E=Orthochromatic erythroblast, Erythrocyte, Promegakaryocyte, Megakaryocyte, Platelet
Some leukocytes migrate into the tissues of the body to take up a
permanent residence at that location rather than remaining in the blood.
Often these cells have specific names depending upon which tissue they
settle in, such as fixed macrophages in the liver, which become known as
Kupffer cells. These cells still serve a role in the immune system.
- Histiocytes
- Dendritic cells (Although these will often migrate to local lymph nodes upon ingesting antigens)
- Mast cells
- Microglia













0 komentar:
Posting Komentar