: Most upper respiratory infections are of viral etiology.
Epiglottitis and laryngotracheitis are exceptions with severe cases likely
caused by
type b. Bacterial pharyngitis
is often caused by Streptococcus pyogenes
: Organisms gain entry to the respiratory tract by
inhalation of droplets and invade the mucosa. Epithelial destruction may ensue,
along with redness, edema, hemorrhage and sometimes an exudate.
: Initial symptoms of a cold are runny,
stuffy nose and sneezing, usually without fever. Other upper respiratory
infections may have fever. Children with epiglottitis may have difficulty in
breathing, muffled speech, drooling and stridor. Children with serious
laryngotracheitis (croup) may also have tachypnea, stridor and cyanosis.
: Common colds can usually be recognized
clinically. Bacterial and viral cultures of throat swab specimens are used for
pharyngitis, epiglottitis and laryngotracheitis. Blood cultures are also
obtained in cases of epiglottitis.
: Viral infections are treated
symptomatically. Streptococcal pharyngitis and epiglottitis caused by
are treated with antibacterials.
type b vaccine is commercially available and is now a
basic component of childhood immunization program.
2. Lower Respiratory Infections: Bronchitis, Bronchiolitis and
Pneumonia
Etiology: Causative agents of lower respiratory infections are viral
or bacterial. Viruses cause most cases of bronchitis and bronchiolitis. In
community-acquired pneumonias, the most common bacterial agent is
Streptococcus pneumoniae. Atypical pneumonias are cause by
such agents as
Mycoplasma pneumoniae, Chlamydia spp, Legionella,
Coxiella burnetti and viruses. Nosocomial pneumonias and pneumonias
in immunosuppressed patients have protean etiology with gram-negative organisms
and staphylococci as predominant organisms.
Pathogenesis: Organisms enter the distal airway by inhalation,
aspiration or by hematogenous seeding. The pathogen multiplies in or on the
epithelium, causing inflammation, increased mucus secretion, and impaired
mucociliary function; other lung functions may also be affected. In severe
bronchiolitis, inflammation and necrosis of the epithelium may block small
airways leading to airway obstruction.
Clinical Manifestations: Symptoms include cough, fever, chest pain,
tachypnea and sputum production. Patients with pneumonia may also exhibit
non-respiratory symptoms such as confusion, headache, myalgia, abdominal pain,
nausea, vomiting and diarrhea.
Microbiologic Diagnosis: Sputum specimens are cultured for bacteria,
fungi and viruses. Culture of nasal washings is usually sufficient in infants
with bronchiolitis. Fluorescent staining technic can be used for legionellosis.
Blood cultures and/or serologic methods are used for viruses, rickettsiae, fungi
and many bacteria. Enzyme-linked immunoassay methods can be used for detections
of microbial antigens as well as antibodies. Detection of nucleotide fragments
specific for the microbial antigen in question by DNA probe or polymerase chain
reaction can offer a rapid diagnosis.
Prevention and Treatment: Symptomatic treatment is used for most
viral infections. Bacterial pneumonias are treated with antibacterials. A
polysaccharide vaccine against 23 serotypes of
Streptococcus
pneumoniae is recommended for individuals at high risk.
Upper Respiratory Infections
Infections of the respiratory tract are grouped according to their symptomatology and
anatomic involvement. Acute upper respiratory infections (URI) include the common
cold, pharyngitis, epiglottitis, and laryngotracheitis. These infections are usually benign, transitory
and self-limited, altho ugh epiglottitis and laryngotracheitis can be serious
diseases in children and young infants. Etiologic agents associated with URI include
viruses, bacteria, mycoplasma and fungi. Respiratory infections are more common in the fall and winter when
school starts and indoor crowding facilitates transmission.

Common Cold
Etiology
Common colds are the most prevalent entity of all respiratory infections and are
the leading cause of patient visits to the physician, as well as work and school
absenteeism. Most colds are caused by viruses. Rhinoviruses with more than 100
serotypes are the most common pathogens, causing at least 25% of colds in
adults. Coronaviruses may be responsible for more than 10% of cases.
Parainfluenza viruses, respiratory syncytial virus, adenoviruses and influenza
viruses have all been linked to the common cold syndrome. All of these organisms
show seasonal variations in incidence. The cause of 30% to 40% of cold syndromes
has not been determined.
Pathogenesis
The viruses appear to act through direct invasion of epithelial cells of the
respiratory mucosa, but
whether there is actual destruction and sloughing of these cells or loss of
ciliary activity depends on the specific organism involved. There is an increase
in both leukocyte infiltration and nasal secretions, including large amounts of
protein and immunoglobulin, suggesting that cytokines and immune mechanisms may
be responsible for some of the manifestations of the common cold.

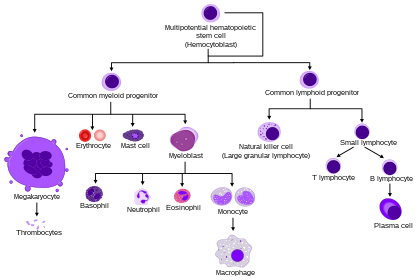
Pathogenesis of viral and bacterial mucosal respiratory
infections.

Pathogenesis of upper respiratory tract infections.
Clinical Manifestations
After an incubation period of 48–72 hours, classic symptoms of nasal
discharge and obstruction, sneezing, sore throat and cough occur in both adults
and children. Myalgia and headache may also be present. Fever is rare. The
duration of symptoms and of viral shedding varies with the pathogen and the age
of the patient. Complications are usually rare, but sinusitis and otitis media
may follow.
Microbiologic Diagnosis
The diagnosis of a common cold is usually based on the symptoms (lack of fever
combined with symptoms of localization to the nasopharynx). Unlike allergic
rhinitis, eosinophils are absent in nasal secretions. Although it is possible to
isolate the viruses for definitive diagnosis, that is rarely warranted.
Prevention and Treatment
Treatment of the uncomplicated common cold is generally symptomatic.
Decongestants, antipyretics, fluids and bed rest usually suffice. Restriction of
activities to avoid infecting others, along with good hand washing, are the best
measures to prevent spread of the disease. No vaccine is commercially available
for cold prophylaxis.
Sinusitis
Sinusitis is an acute inflammatory condition of one or more of the paranasal
sinuses. Infection plays an important role in this affliction. Sinusitis often
results from infections of other sites of the respiratory tract since the
paranasal sinuses are contiguous to, and communicate with, the upper respiratory
tract.
Etiology
Acute sinusitis most often follows a common cold which is usually of viral
etiology. Vasomotor and allergic rhinitis may also be antecedent to the
development of sinusitis. Obstruction of the sinusal ostia due to deviation of
the nasal septum, presence of foreign bodies, polyps or tumors can predispose to
sinusitis. Infection of the maxillary sinuses may follow dental extractions or
an extension of infection from the roots of the upper teeth. The most common
bacterial agents responsible for acute sinusitis are Streptococcus
pneumoniae, Haemophilus influenzae, and Moraxella
catarrhalis. Other organisms including Staphylococcus
aureus, Streptococcus pyogenes, gram-negative organisms and
anaerobes have also been recovered. Chronic sinusitis is commonly a mixed
infection of aerobic and anaerobic organisms.
Pathogenesis
Infections caused by viruses or bacteria impair the ciliary activity of the
epithelial lining of the sinuses and increased mucous secretions. This leads to
obstruction of the paranasal sinusal ostia which impedes drainage. With
bacterial multiplication in the sinus cavities, the mucus is converted to
mucopurulent exudates. The pus further irritates the mucosal lining causing more
edema, epithelial destruction and ostial obstruction. When acute sinusitis is
not resolved and becomes chronic, mucosal thickening results and the development
of mucoceles and polyps may ensue.
Clinical Manifestations
The maxillary and ethmoid sinuses are most commonly involved in sinusitis. The
frontal sinuses are less often involved and the sphenoid sinuses are rarely
affected. Pain, sensation of pressure and tenderness over the affected sinus are
present. Malaise and low grade fever may also occur. Physical examination
usually is not remarkable with no more than an edematous and hyperemic nasal
mucosa.
In uncomplicated chronic sinusitis, a purulent nasal discharge is the most
constant finding. There may not be pain nor tenderness over the sinus areas.
Thickening of the sinus mucosa and a fluid level are usually seen in x-ray films
or magnetic resonance imaging.
Microbiologic Diagnosis
For acute sinusitis, the diagnosis is made from clinical findings. A bacterial
culture of the nasal discharge can be taken but is not very helpful as the
recovered organisms are generally contaminated by the resident flora from the
nasal passage. In chronic sinusitis, a careful dental examination, with sinus
x-rays may be required. An antral puncture to obtain sinusal specimens for
bacterial culture is needed to establish a specific microbiologic diagnosis.
Prevention and Treatment
Symptomatic treatment with analgesics and moist heat over the affected sinus pain
and a decongestant to promote sinus drainage may suffice. For antimicrobial
therapy, a beta-lactamase resistant antibiotic such as amoxicillin-clavulanate
or a cephalosporin may be used. For chronic sinusitis, when conservative
treatment does not lead to a cure, irrigation of the affected sinus may be
necessary. Culture from an antral puncture of the maxillary sinus can be
performed to identify the causative organism for selecting antimicrobial
therapy. Specific preventive procedures are not available. Proper care of
infectious and/or allergic rhinitis, surgical correction to relieve or avoid
obstruction of the sinusal ostia are important. Root abscesses of the upper
teeth should receive proper dental care to avoid secondary infection of the
maxillary sinuses.
Otitis
Infections of the ears are common events encountered in medical practice,
particularly in young children. Otitis externa is an infection involving the
external auditory canal while otitis media denotes inflammation of the middle
ear.
Etiology
For otitis externa, the skin flora such as Staphylococcus epidermidis,
Staphylococcus aureus, diphtheroids and occasionally an anaerobic
organism, Propionibacterium acnes are major etiologic agents.
In a moist and warm environment, a diffuse acute otitis externa (Swimmer's ear)
may be caused by Pseudomonas aeruginosa, along with other skin
flora. Malignant otitis externa is a severe necrotizing infection usually caused
by Pseudomonas aeruginosa.
For otitis media, the commonest causative bacteria are Streptococcus
pneumoniae, Hemophilus influenzae and beta-lactamase producing
Moraxella catarrhalis. Respiratory viruses may play a role
in otitis media but this remains uncertain. Mycoplasma
pneumoniae has been reported to cause hemorrhagic bullous
myringitis in an experimental study among nonimmune human volunteers inoculated
with M pneumoniae. However, in natural cases of M
pneumoniae infection, clinical bullous myringitis or otitis media
is uncommon.
Pathogenesis
The narrow and tortuous auditory canal is lined by a protective surface
epithelium. Factors that may disrupt the natural protective mechanisms, such as
high temperature and humidity, trauma, allergy, tissue maceration, removal of
cerumen and an alkaline pH environment, favor the development of otitis externa.
Prolonged immersion in a swimming pool coupled with frequent ear cleansing
increases the risk of otitis externa.
Acute otitis media commonly follows an upper respiratory infection extending from
the nasopharynx via the eustachian tube to the middle ear. Vigorous nose blowing
during a common cold, sudden changes of air pressure, and perforation of the
tympanic membrane also favor the development of otitis media. The presence of
purulent exudate in the middle ear may lead to a spread of infection to the
inner ear and mastoids or even meninges
Clinical Manifestations
Otitis externa
Furuncles of the external ear, similar to those in skin infection, can cause
severe pain and a sense of fullness in the ear canal. When the furuncle
drains, purulent otorrhea may be present. In generalized otitis externa,
itching, pain and tenderness of the ear lobe on traction are present. Loss
of hearing may be due to obstruction of the ear canal by swelling and the
presence of purulent debris.
Malignant otitis externa tends to occur in elderly diabetic patients. It is
characterized by severe persistent earache, foul smelling purulent discharge
and the presence of granulation tissue in the auditory canal. The infection
may spread and lead to osteomyelitis of the temporal bone or externally to
involve the pinna with osteochondritis.
Otitis media
Acute otitis media occurs most commonly in young children. The initial
complaint usually is persistent severe earache (crying in the infant)
accompanied by fever, and, and vomiting. Otologic examination reveals a
bulging, erythematous tympanic membrane with loss of light reflex and
landmarks. If perforation of the tympanic membrane occurs, serosanguinous or
purulent discharge may be present. In the event of an obstruction of the
eustachian tube, accumulation of a usually sterile effusion in the middle
ear results in serous otitis media. Chronic otitis media frequently presents
a permanent perforation of the tympanic membrane. A central perforation of
the pars tensa is more benign. On the other hand, an attic perforation of
the pars placcida and marginal perforation of the pars tensa are more
dangerous and often associated with a cholesteatoma.
Diagnosis
The diagnosis of both otitis externa and otitis media can be made from history,
clinical symptomatology and physical examinations. Inspection of the tympanic
membrane is an indispensable skill for physicians and health care workers. All
discharge, ear wax and debris must be removed and to perform an adequate
otoscopy. In the majority of patients, routine cultures are not necessary, as a
number of good bacteriologic studies have shown consistently the same microbial
pathogens mentioned in the section of etiology. If the patient is
immunocompromised or is toxic and not responding to initial antimicrobial
therapy tympanocentesis (needle aspiration) to obtain middle ear effusion for
microbiologic culture is indicated.
Prevention and Treatment
Otitis externa
Topical therapy is usually sufficient and systemic antimicrobials are seldom
needed unless there are signs of spreading cellulitis and the patient
appears toxic. A combination of topical antibiotics such as neomycin
sulfate, polymyxin B sulfate and corticosteroids used as eardrops, is a
preferred therapy. In some cases, acidification of the ear canal by applying
a 2% solution of acetic acid topically may also be effective. If a furuncle
is present in the external canal, the physician should allow it to drain
spontaneously.
Otitis media
Amoxicillin is an effective and preferred antibiotic for treatment of acute
otitis media. Since beta-lactamase producing H influenzae
and M catarrhalis can be a problem in some communities,
amoxicillin-clavulanate is used by many physicians. Oral preparations of
trimethoprim/sulfamethoxazole, second and third generation cephalosporins,
tetracyclines and macrolides can also be used. When there is a large
effusion, tympanocentesis may hasten the resolution process by decreasing
the sterile effusion. Patients with chronic otitis media and frequent
recurrences of middle ear infections may be benefitted by chemoprophylaxis
with once daily oral amoxicillin or trimethoprim/sulfamethoxazole during the
winter and spring months. In those patients with persistent effusion of the
middle ear, surgical interventions with myringotomy, adenoidectomy and the
placement of tympanotomy tubes has been helpful.
Use of polyvalent pneumococcal vaccines has been evaluated for the prevention
of otitis media in children. However, children under two years of age do not
respond satisfactorily to polysaccharide antigens; further, no significant
reduction in the number of middle ear infections was demonstrable. Newer
vaccines composed of pneumococcal capsular polysaccharides conjugated to
proteins may increase the immunogenicity and are currently under clinical
investigation for efficacy and safety.
Pharyngitis
Etiology
Pharyngitis is an inflammation of the pharynx involving lymphoid tissues of the
posterior pharynx and lateral pharyngeal bands. The etiology can be bacterial,
viral and fungal infections as well as noninfectious etiologies such as smoking.
Most cases are due to viral infections and accompany a common cold or influenza.
Type A coxsackieviruses can cause a severe ulcerative pharyngitis in children
(herpangina), and adenovirus and herpes simplex virus, although less common,
also can cause severe pharyngitis. Pharyngitis is a common symptom of
Epstein-Barr virus and cytomegalovirus infections.
Group A beta-hemolytic streptococcus or Streptococcus pyogenes
is the most important bacterial agent associated with acute pharyngitis and
tonsillitis. Corynebacterium diphtheriae causes occasional
cases of acute pharyngitis, as do mixed anaerobic infections (Vincent's angina),
Corynebacterium haemolyticum, Neisseria gonorrhoeae, and
Chlamydia trachomatis. Outbreaks of Chlamydia
pneumoniae (TWAR agent) causing pharyngitis or pneumonitis have
occurred in military recruits. Mycoplasma pneumoniae and
Mycoplasma hominis have been associated with acute
pharyngitis. Candida albicans, which causes oral candidiasis or
thrush, can involve the pharynx, leading to inflammation and pain.
Pathogenesis
As with common cold, viral pathogens in pharyngitis appear to invade the mucosal
cells of the nasopharynx and oral cavity, resulting in edema and hyperemia of
the mucous membranes and tonsils (). Bacteria attach to and, in the case of group A beta-hemolytic
streptococci, invade the mucosa of the upper respiratory tract. Many clinical
manifestations of infection appear to be due to the immune reaction to products
of the bacterial cell. In diphtheria, a potent bacterial exotoxin causes local
inflammation and cell necrosis.
Clinical Manifestations
Pharyngitis usually presents with a red, sore, or “scratchy”
throat. An inflammatory exudate or membranes may cover the tonsils and tonsillar
pillars. Vesicles or ulcers may also be seen on the pharyngeal walls. Depending
on the pathogen, fever and systemic manifestations such as malaise, myalgia, or
headache may be present. Anterior cervical lymphadenopathy is common in
bacterial pharyngitis and difficulty in swallowing may be present.
Microbiologic Diagnosis
The goal in the diagnosis of pharyngitis is to identify cases that are due to
group A beta-hemolytic streptococci, as well as the more unusual and potentially
serious infections. The various forms of pharyngitis cannot be distinguished on
clinical grounds. Routine throat cultures for bacteria are inoculated onto sheep
blood and chocolate agar plates. Thayer-Martin medium is used if N
gonorrhoeae is suspected. Viral cultures are not routinely obtained
for most cases of pharyngitis. Serologic studies may be used to confirm the
diagnosis of pharyngitis due to viral, mycoplasmal or chlamydial pathogens.
Rapid diagnostic tests with fluorescent antibody or latex agglutination to
identify group A streptococci from pharyngeal swabs are available. Gene probe
and polymerase chain reaction can be used to detect unusual organisms such as
M pneumoniae, chlamydia or viruses but these procedures are
not routine diagnostic methods.
Prevention and Treatment
Symptomatic treatment is recommended for viral pharyngitis. The exception is
herpes simplex virus infection, which can be treated with acyclovir if
clinically warranted or if diagnosed in immunocompromised patients. The specific
antibacterial agents will depend on the causative organism, but penicillin G is
the therapy of choice for streptococcal pharyngitis. Mycoplasma and chlamydial
infections respond to erythromycin, tetracyclines and the new macrolides.
Epiglottitis and Laryngotracheitis
Etiology
Inflammation of the upper airway is classified as epiglottitis or
laryngotracheitis (croup) on the basis of the location, clinical manifestations,
and pathogens of the infection. Haemophilus influenzae type b
is the most common cause of epiglottitis, particularly in children age 2 to 5
years. Epiglottitis is less common in adults. Some cases of epiglottitis in
adults may be of viral origin. Most cases of laryngotracheitis are due to
viruses. More serious bacterial infections have been associated with H
influenzae type b, group A beta-hemolytic streptococcus and
C diphtheriae. Parainfluenza viruses are most common but
respiratory syncytial virus, adenoviruses, influenza viruses, enteroviruses and
Mycoplasma pneumoniae have been implicated.
Pathogenesis
A viral upper respiratory infection may precede infection with H
influenzae in episodes of epiglottitis. However, once H
influenzae type b infection starts, rapidly progressive erythema
and swelling of the epiglottis ensue, and bacteremia is usually present. Viral
infection of laryngotracheitis commonly begins in the nasopharynx and eventually
moves into the larynx and trachea. Inflammation and edema involve the
epithelium, mucosa and submucosa of the subglottis which can lead to airway
obstruction.
Clinical Manifestations
The syndrome of epiglottitis begins with the acute onset of fever, sore throat,
hoarseness, drooling, dysphagia and progresses within a few hours to severe
respiratory distress and prostration. The clinical course can be fulminant and
fatal. The pharynx may be inflamed, but the diagnostic finding is a
“cherry-red” epiglottis.
A history of preceding cold-like symptoms is typical of laryngotracheitis, with
rhinorrhea, fever, sore throat and a mild cough. Tachypnea, a deep barking cough
and inspiratory stridor eventually develop. Children with bacterial tracheitis
appear more ill than adults and are at greater risk of developing airway
obstruction.
Haemophilus influenzae type b is isolated from the blood or
epiglottis in the majority of patients with epiglottis; therefore a blood
culture should always be performed. Sputum cultures or cultures from pharyngeal
swabs may be used to isolate pathogens in patients with laryngotracheitis.
Serologic studies to detect a rise in antibody titers to various viruses are
helpful for retrospective diagnosis. Newer, rapid diagnostic techniques, using
immunofluorescent-antibody staining to detect virus in sputum, pharyngeal swabs,
or nasal washings, have been successfully used. Enzyme-linked immunosorbent
assay (ELISA), DNA probe and polymerase chain reaction procedures for detection
of viral antibody or antigens are now available for rapid diagnosis.
Prevention and Treatment
Epiglottitis is a medical emergency, especially in children. All children with
this diagnosis should be observed carefully and be intubated to maintain an open
airway as soon as the first sign of respiratory distress is detected.
Antibacterial therapy should be directed at H influenzae.
Patients with croup are usually successfully managed with close observation and
supportive care, such as fluid, humidified air, and racemic epinephrine. For
prevention, Haemophilus influenzae type b conjugated vaccine is
recommended for all pediatric patients, as is immunization against
diphtheria.
Lower Respiratory Infections
Infections of the lower respiratory tract include bronchitis, bronchiolitis and
pneumonia. These syndromes,
especially pneumonia, can be severe or fatal. Although viruses, mycoplasma,
rickettsiae and fungi can all cause lower respiratory tract infections, bacteria
are the dominant pathogens; accounting for a much higher percentage of lower
than of upper respiratory tract infections.
Bronchitis and Bronchiolitis
Etiology
Bronchitis and bronchiolitis involve inflammation of the bronchial tree.
Bronchitis is usually preceded by an upper respiratory tract infection or forms
part of a clinical syndrome in diseases such as influenza, rubeola, rubella,
pertussis, scarlet fever and typhoid fever. Chronic bronchitis with a persistent
cough and sputum production appears to be caused by a combination of
environmental factors, such as smoking, and bacterial infection with pathogens
such as H influenzae and S pneumoniae.
Bronchiolitis is a viral respiratory disease of infants and is caused primarily
by respiratory syncytial virus. Other viruses, including parainfluenza viruses,
influenza viruses and adenoviruses (as well as occasionally M
pneumoniae) are also known to cause bronchiolitis.
Pathogenesis
When the bronchial tree is infected, the mucosa becomes hyperemic and edematous
and produces copious bronchial secretions. The damage to the mucosa can range
from simple loss of mucociliary function to actual destruction of the
respiratory epithelium, depending on the organisms(s) involved. Patients with
chronic bronchitis have an increase in the number of mucus-producing cells in
their airways, as well as inflammation and loss of bronchial epithelium, Infants
with bronchiolitis initially have inflammation and sometimes necrosis of the
respiratory epithelium, with eventual sloughing. Bronchial and bronchiolar walls
are thickened. Exudate made up of necrotic material and respiratory secretions
and the narrowing of the bronchial lumen lead to airway obstruction. Areas of
air trapping and atelectasis develop and may eventually contribute to
respiratory failure.
Clinical Manifestations
Symptoms of an upper respiratory tract infection with a cough is the typical
initial presentation in acute bronchitis. Mucopurulent sputum may be present,
and moderate temperature elevations occur. Typical findings in chronic
bronchitis are an incessant cough and production of large amounts of sputum,
particularly in the morning. Development of respiratory infections can lead to
acute exacerbations of symptoms with possibly severe respiratory distress.
Coryza and cough usually precede the onset of bronchiolitis. Fever is common. A
deepening cough, increased respiratory rate, and restlessness follow.
Retractions of the chest wall, nasal flaring, and grunting are prominent
findings. Wheezing or an actual lack of breath sounds may be noted. Respiratory
failure and death may result.
Microbiologic Diagnosis
Bacteriologic examination and culture of purulent respiratory secretions should
always be performed for cases of acute bronchitis not associated with a common
cold. Patients with chronic bronchitis should have their sputum cultured for
bacteria initially and during exacerbations. Aspirations of nasopharyngeal
secretions or swabs are sufficient to obtain specimens for viral culture in
infants with bronchiolitis. Serologic tests demonstrating a rise in antibody
titer to specific viruses can also be performed. Rapid diagnostic tests for
antibody or viral antigens may be performed on nasopharyngeal secretions by
using fluorescent-antibody staining, ELISA or DNA probe procedures.
Prevention and Treatment
With only a few exceptions, viral infections are treated with supportive
measures. Respiratory syncytial virus infections in infants may be treated with
ribavirin. Amantadine and rimantadine are available for chemoprophylaxis or
treatment of influenza type A viruses. Selected groups of patients with chronic
bronchitis may receive benefit from use of corticosteroids, bronchodilators, or
prophylactic antibiotics.
Pneumonia
Pneumonia is an inflammation of the lung parenchyma. Consolidation of the lung tissue may be
identified by physical examination and chest x-ray. From an anatomical point of
view, lobar pneumonia denotes an alveolar process involving an entire lobe of
the lung while bronchopneumonia describes an alveolar process occurring in a
distribution that is patchy without filling an entire lobe. Numerous factors,
including environmental contaminants and autoimmune diseases, as well as
infection, may cause pneumonia. The various infectious agents that cause
pneumonia are categorized in many ways for purposes of laboratory testing,
epidemiologic study and choice of therapy. Pneumonias occurring in usually
healthy persons not confined to an institution are classified as
community-acquired pneumonias. Infections arise while a patient is hospitalized
or living in an institution such as a nursing home are called hospital-acquired
or nosocomial pneumonias. Etiologic pathogens associated with community-acquired
and hospital-acquired pneumonias are somewhat different. However, many organisms
can cause both types of infections.

Pathogenesis of bacterial pneumonias.
Etiology
Bacterial pneumonias
Streptococcus pneumoniae is the most common agent of
community-acquired acute bacterial pneumonia. More than 80 serotypes, as
determined by capsular polysaccharides, are known, but 23 serotypes account
for over 90% of all pneumococcal pneumonias in the United States. Pneumonias
caused by other streptococci are uncommon. Streptococcus
pyogenes pneumonia is often associated with a hemorrhagic
pneumonitis and empyema. Community-acquired pneumonias caused by
Staphylococcus aureus are also uncommon and usually
occur after influenza or from staphylococcal bacteremia. Infections due to
Haemophilus influenzae (usually nontypable) and
Klebsiella pneumoniae are more common among patients
over 50 years old who have chronic obstructive lung disease or
alcoholism.
The most common agents of nosocomial pneumonias are aerobic gram-negative
bacilli that rarely cause pneumonia in healthy individuals.
Pseudomonas aeruginosa, Escherichia coli, Enterobacter,
Proteus, and Klebsiella species are often
identified. Less common agents causing pneumonias include
Francisella tularensis, the agent of tularemia;
Yersinia pestis, the agent of plague; and
Neisseria meningitidis, which usually causes meningitis
but can be associated with pneumonia, especially among military recruits.
Xanthomonas pseudomallei causes melioidosis, a chronic
pneumonia in Southeast Asia.
Mycobacterium tuberculosis can cause pneumonia. Although the
incidence of tuberculosis is low in industrialized countries, M
tuberculosis infections still continue to be a significant
public health problem in the United States, particularly among immigrants
from developing countries, intravenous drug abusers, patients infected with
human immunodeficiency virus (HIV), and the institutionalized elderly.
Atypical Mycobacterium species can cause lung disease
indistinguishable from tuberculosis.
Aspiration pneumonias
Aspiration pneumonia from anaerobic organisms usually occurs in patients with
periodontal disease or depressed consciousness. The bacteria involved are
usually part the oral flora and cultures generally show a mixed bacterial
growth. Actinomyces, Bacteroides, Peptostreptococcus, Veilonella,
Propionibacterium, Eubacterium, and
Fusobacterium spp are often isolated.
Atypical pneumonias
Atypical pneumonias are those that are not typical bacterial lobar
pneumonias. Mycoplasma pneumoniae produces pneumonia most
commonly in young people between 5 and 19 years of age. Outbreaks have been
reported among military recruits and college students.
Legionella species, including L pneumophila, can cause a
wide range of clinical manifestations. The 1976 outbreak in Philadelphia was
manifested as a typical serious pneumonia in affected individuals, with a
mortality of 17%.
These organisms can survive in water and cause pneumonia by inhalation from
aerosolized tap water, respiratory devices, air conditioners and showers.
They also have been reported to cause nosocomial pneumonias.
Chlamydia spp noted to cause pneumonitis are C
trachomatis, C psittaci and C pneumoniae.
Chlamydia trachomatis causes pneumonia in neonates and
young infants. C psittaci is a known cause for occupational
pneumonitis in bird handlers such as turkey farmers. Chlamydia
pneumoniae has been associated with outbreaks of pneumonia in
military recruits and on college campuses.
Coxiella burnetii the rickettsia responsible for Q fever, is
acquired by inhalation of aerosols from infected animal placentas and feces.
Pneumonitis is one of the major manifestations of this systemic
infection.
Viral pneumonias are rare in healthy civilian adults. An exception is the
viral pneumonia caused by influenza viruses, which can have a high mortality
in the elderly and in patients with underlying disease. A serious
complication following influenza virus infection is a secondary bacterial
pneumonia, particularly staphylococcal pneumonia. Respiratory syncytial
virus can cause serious pneumonia among infants as well as outbreaks among
institutionalized adults. Adenoviruses may also cause pneumonia, serotypes
1,2,3,7 and 7a have been associated with a severe, fatal pneumonia in
infants. Although varicella-zoster virus pneumonitis is rare in children, it
is not uncommon in individuals over 19 years old. Morality can be as high as
10% to 30%. Measles pneumonia may occur in adults.
Other pneumonias and immunosuppression
Cytomegalovirus is well known for causing congenital infections in neonates,
as well as the mononucleosis-like illness seen in adults. However, among its
manifestations in immunocompromised individuals is a severe and often fatal
pneumonitis. Herpes simplex virus also causes a pneumonia in this
population. Giant-cell pneumonia is a serious complication of measles and
has been found in children with immunodeficiency disorders or underlying
cancers who receive live attenuated measles vaccine.
Actinomyces and Nocardia spp can cause
pneumonitis, particularly in immunocompromised hosts.
Among the fungi, Cryptococcus neoformans and
Sporothrix schenckii are found worldwide, whereas
Blastomyces dermatitidis, Coccidioides immitis, Histoplasma
capsulatum and Paracoccidioides brasiliensis
have specific geographic distributions. All can cause pneumonias, which are
usually chronic and possible clinically inapparent in normal hosts, but are
manifested as more serious diseases in immunocompromised patients. Other
fungi, such as Aspergillus and Candida
spp, occasionally are responsible for pneumonias in severely ill or
immunosuppressed patients and neonates.
Pneumocystis carinii produces a life-threatening pneumonia
among patients immunosuppressed by acquired immune deficiency syndrome
(AIDS), hematologic cancers, or medical therapy. It is the most common cause
of pneumonia among patients with AIDS when the CD4 cell counts drop below
200/mm3.
Pathogenesis and Clinical Manifestations
Infectious agents gain access to the lower respiratory tract by the inhalation of
aerosolized material, by aspiration of upper airway flora, or by hematogenous
seeding. Pneumonia occurs when lung defense mechanisms are diminished or
overwhelmed. The major symptoms or pneumonia are cough, chest pain, fever,
shortness of breath and sputum production. Patients are tachycardic. Headache,
confusion, abdominal pain, nausea, vomiting and diarrhea may be present,
depending on the age of the patient and the organisms involved.
Microbiologic Diagnosis
Etiologic diagnosis of pneumonia on clinical grounds alone is almost impossible.
Sputum should be examined for a predominant organism in any patient suspected to
have a bacterial pneumonia; blood and pleural fluid (if present) should be
cultured. A sputum specimen with fewer than 10 while cells per high-power field
under a microscope is considered to be contaminated with oral secretions and is
unsatisfactory for diagnosis. Acid-fast stains and cultures are used to identify
Mycobacterium and Nocardia spp. Most
fungal pneumonias are diagnosed on the basis of culture of sputum or lung
tissue. Viral infection may be diagnosed by demonstration of antigen in
secretions or cultures or by an antibody response. Serologic studies can be used
to identify viruses, M pneumoniae, C. burnetii, Chlamydia species,
Legionella, Francisella, and Yersinia. A rise in
serum cold agglutinins may be associated with M pneumoniae
infection, but the test is positive in only about 60% of patients with this
pathogen.
Rapid diagnostic tests, as described in previous sections, are available to
identify respiratory viruses: the fluorescent-antibody test is used for
Legionella. A sputum quellung test can specify S
pneumoniae by serotype. Enzyme-linked immunoassay, DNA probe and
polymerase chain reaction methods are available for many agents causing
respiratory infections.
Some organisms that may colonize the respiratory tract are considered to be
pathogens only when they are shown to be invading the parenchyma. Diagnosis of
pneumonia due to cytomegalovirus, herpes simplex virus,
Aspergillus spp. or Candida spp require
specimens obtained by transbronchial or open-lung biopsy. Pneumocystis
carinii can be found by silver stain of expectorated sputum.
However, if the sputum is negative, deeper specimens from the lower respiratory
tract obtained by bronchoscopy or by lung biopsy are needed for confirmatory
diagnosis.
Prevention and Treatment
Until the organism causing the infection is identified, decisions on therapy are
based upon clinical history, including history of exposure, age, underlying
disease and previous therapies, past pneumonias, geographic location, severity
of illness, clinical symptoms, and sputum examination. Once a diagnosis is made,
therapy is directed at the specific organism responsible.
The pneumococcal vaccine should be given to patients at high risk for developing
pneumococcal infections, including asplenic patients, the elderly and any
patients immunocompromised through disease or medical therapy. Yearly influenza
vaccinations should also be provided for these particular groups. An
enteric-coated vaccine prepared from certain serotypes of adenoviruses is
available, but is only used in military recruits. In AIDS patients,
trimethoprim/sulfamethoxazole, aerosolized pentamidine or other antimicrobials
can be given for prophylaxis of Pneumocystis carinii
infections.